
Regarding health problems, iliotibial band syndrome (ITBS) is one of the most frequent and treatable in many ways. This blog will provide information and advice on how to deal with ITBS. We’ll also discuss the different treatments available. Read on to find out!
Description Of Iliotibial Band
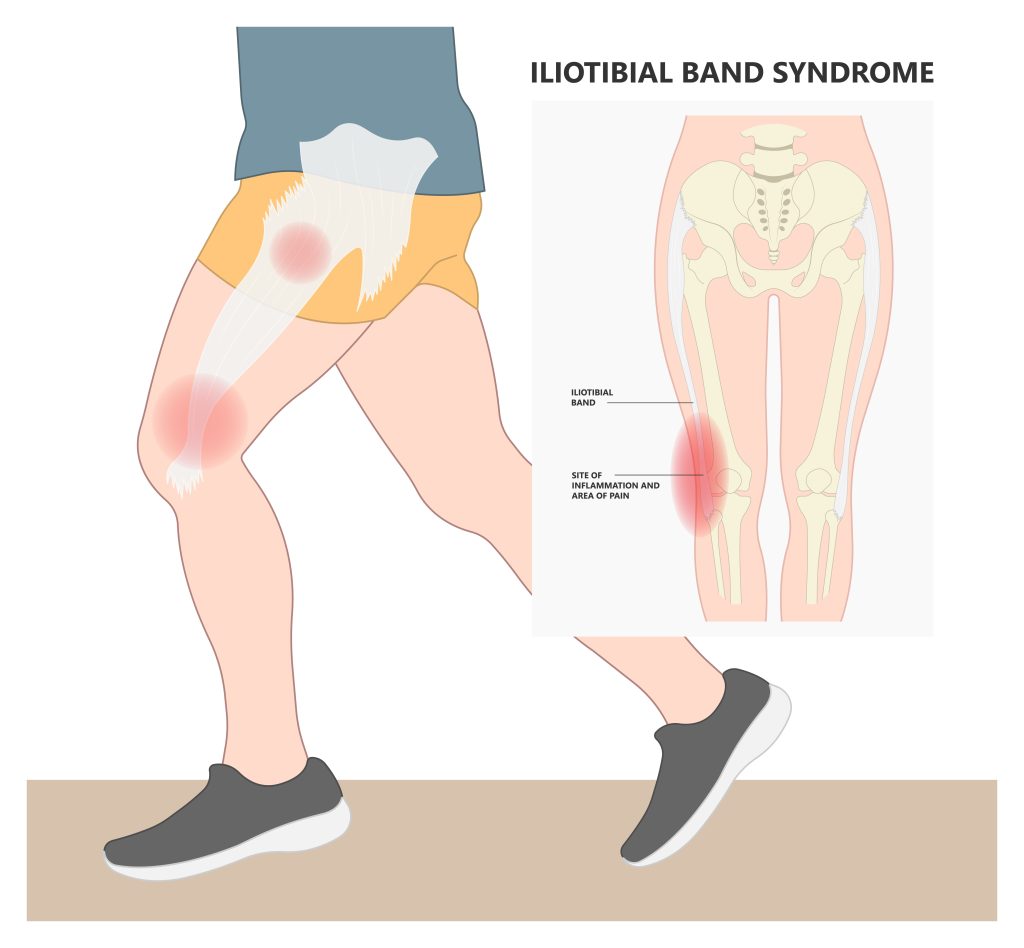
The outer side of your thigh has a thick, fibrous band of tissue known as the iliotibial band. It extends from your hip down to the top of your kneecap and connects to the hip, knee, and lower leg. It connects to muscles inside your leg and helps stabilize your knee joint while you move. When the iliotibial band becomes inflamed, it can cause pain in your knee or hip. This condition is called iliotibial band syndrome or ITBS.
What is ITB Syndrome?
ITBS occurs when there’s friction between the ITB and the boney side of your knee joint. It’s also sometimes called iliotibial band friction syndrome or ITBFS. This friction causes inflammation, swelling, and pain in your ITB. This rubbing occurs by excessive pressure on the area. This includes running, walking uphill, downhill slopes, cycling, jumping rope, squats, or lunges.
Who is most commonly affected by ITBS?
ITBS most often affects physically active people. Examples include runners, cyclists, hikers, and military personnel. It can also affect those who participate in sports like basketball and soccer.
Causes of ITBS
The exact cause of ITBS isn’t known. Still, tightness in your iliotibial band can cause friction in your knee joint. Tight muscles may also pull on the bone, causing inflammation and pain.
The ITB can become inflamed in several ways:
- Overuse from running or cycling too much, especially on hilly terrain.
- Tightness in your hips or glutes (butt muscles), which can cause imbalanced forces at the knee.
- Pronation, or rolling inward with each step you take. This activity causes increased stress on the ITB when it rubs against bone.
- Tightness in other muscles around your knees, including quadriceps and hamstrings. Tight muscles can pull on the ITB and cause inflammation or irritation over time.
You should see a doctor if the pain persists for more than two weeks after starting treatment.
Symptoms of ITBS
If you have iliotibial band syndrome, your symptoms include:
- Pain on the outside of your knee that gets worse when you walk or run.
- Tenderness or swelling near the place where the iliotibial band attaches to the knee.
- A popping or snapping sensation in your knee when you move it. Especially when you run or sit with your legs crossed.
- Worsening symptoms with prolonged periods of sitting or standing still.
How to diagnose ITBS?
The diagnosis typically depends on the history, physical exam, and imaging studies. It can be challenging to distinguish ITBS from other causes of lateral knee pain.

Ideally, you should see an orthopedist or your primary care doctor if you think you have it. They will likely perform an examination and order an X-ray or MRI scan. This lab examination helps them determine the cause of your pain. They will differentiate ITBS from similar injuries you had with your knees or legs. For example, suppose you are suffering from ITBS but also have a history of arthritis in the knee or hip joints. In that case, there may be another cause for your pain, such as degenerative joint disease. Suppose they find that your symptoms are not consistent with iliotibial band syndrome. In that case, they may suggest a specialist to determine whether there is another cause for your pain.
Your doctor should also do a physical exam to look for signs of injury. They should test for a range of motion (ROM) at both hip and ankle joints. They can also use an ultrasound machine to better look at what’s happening inside your knee joint.
Special Tests used to diagnose ITBS
Noble Compression Test – Hips and knees are passively flexed to 90 degrees. Keeping your thumb over the IT band proximal to the lateral femoral condyle, you actively extend your hips and knees. A positive test means you feel pain over the distal IT band before 30 degrees under knee extension. If it hurts less than 30 degrees, it’s negative.
During Ober’s Test you must be side-lying with your lower leg flexed at the hip and knee to ensure stability. The examiner then passively abducts the upper leg and extends it slightly. At the same time, while fixing the pelvis with the other hand. You need to lower your upper leg slowly down to the table. This test is positive if the upper leg stays in the air and doesn’t fall onto the table.
Treatment of ITBS
- Rest – Some experts recommend resting your injured leg until the pain disappears. Ask your doctor how much rest you should get
- Pain medications – You should talk to your healthcare provider about the proper dosage of (NSAIDs).
- Steroid Injections – It might reduce the inflammation in your iliotibial band.
Physical Therapy Intervention
Physical therapy can help relieve your pain by teaching you exercises and other treatments. These treatments might help you loosen your iliotibial band and decrease the tension. Physical therapists can show you how to warm up before exercise and cool down afterward.
- Manual Therapy – A foam roller for massage is an example of manual therapy.
- Posture Training – Your posture can affect your iliotibial band syndrome when you’re going about your daily life, playing sports, or otherwise.
Alternative Treatments
- Acupuncture boosts your natural healing response. It stimulates the body by inserting needles at specific points. Acupuncture can help reduce inflammation, one of the main causes of ITBS symptoms.
- Kinesiology taping can help relieve pain and inflammation by supporting the area around the injured tissue. It does this by lifting the skin away from the inflamed tissue and reducing pressure on blood vessels and nerves.
Surgery
If you don’t get better with medications and physical therapy, your healthcare provider might recommend surgery.
How to prevent ITBS
Here are some tips for preventing iliotibial band syndrome:
- Stretch before running or working out. By stretching, you’ll loosen up your muscles and prevent them from tightening up during activity.
- Run on softer ground, like grass or sand, instead of concrete sidewalks or asphalt roads.
- Wear proper footwear, including shoes with good arch support and enough padding in certain areas.

A Note From Gulf Physio
We hope you’ve enjoyed learning about the subject matter above. This blog post is not a substitute for medical advice. The author cannot guarantee the accuracy of the information presented. If you have any questions or concerns, please consult a healthcare professional. All decisions and actions you make are your own. No one involved in making this resource is liable for its use.



